Prevention of perioperative AKI, mostly from ATN by ischemic insult, has been a major challenge in nephrology. Recent study (Zarbock et al. JAMA) showed a simple, non-invasive method—remote ischemic preconditioning (RIPC), could be a promising strategy.
This multicenter, double-blind study in Germany randomized 240 patients undergoing on-pump cardiac surgery, who had high risk for AKI (based on Cleveland Clinic Foundation score). Exclusion criteria included eGFR below 30 ml/min or transplant recipient. Intervention consisted of: 3 cycles of 5-minute inflation of a blood pressure cuff to 200 mmHg (or 50 mmHg higher than the systolic pressure) to one upper arm, followed by 5-minute reperfusion with the cuff deflated.
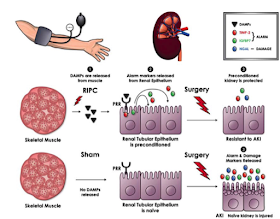
Primary endpoint was the incidence of AKI within 72-hour post-op (KDIGO criteria). They found significantly fewer patients in RIPC group developed AKI (37.5% vs 52.5%; p=0.02; RR, 71% 95% CI, 54-95%). Use of renal replacement therapy was also lower (5.8% vs 15.8%; p=0.01). Of note, the authors examined urine biomarkers: tissue inhibitor of metaloproteinases 2 (TIMP-2) x insulin-like growth factor-binding protein 7 (IGFBP7), as well as urine neutrophil gelatinase-associated lipocalin (NGAL) and high-mobility group box (HMGB). TIMP-2 and IGFBP were measured by Nephrocheck® (see previous blog entry for details). Biproduct of TIMP2 x IGFBP7 and HMGB increased right after RIPC, suggestive of cell cycle arrest as an epithelial defensive mechanism against ischemic insult, however, in 4-24 hours post-op, TIMP2 x IGFBP7 and NGAL were lower in RIPC group compared to control (schematic figure above from eSupplement), indicating less kidney damage.
RIPC has been studied in kidney transplant field as well. The REPAIR trial recruited 406 live donor-recipient pairs and looked into 12-month post-transplant eGFR with or without early or late RIPC for both donors and recipients. The result was not significant, but as Zarbock et al. pointed out in their article, it could be due to differences in study protocols, confounding comorbidities, or surgical technique. Further studies to explain the mechanism of protection is warranted and it might be no exaggeration to say that RIPC would be a standard pre-op protocol for cardiac surgery in the near future. Are your kidneys ready for surgery?
Naoka Murakami
This multicenter, double-blind study in Germany randomized 240 patients undergoing on-pump cardiac surgery, who had high risk for AKI (based on Cleveland Clinic Foundation score). Exclusion criteria included eGFR below 30 ml/min or transplant recipient. Intervention consisted of: 3 cycles of 5-minute inflation of a blood pressure cuff to 200 mmHg (or 50 mmHg higher than the systolic pressure) to one upper arm, followed by 5-minute reperfusion with the cuff deflated.
Primary endpoint was the incidence of AKI within 72-hour post-op (KDIGO criteria). They found significantly fewer patients in RIPC group developed AKI (37.5% vs 52.5%; p=0.02; RR, 71% 95% CI, 54-95%). Use of renal replacement therapy was also lower (5.8% vs 15.8%; p=0.01). Of note, the authors examined urine biomarkers: tissue inhibitor of metaloproteinases 2 (TIMP-2) x insulin-like growth factor-binding protein 7 (IGFBP7), as well as urine neutrophil gelatinase-associated lipocalin (NGAL) and high-mobility group box (HMGB). TIMP-2 and IGFBP were measured by Nephrocheck® (see previous blog entry for details). Biproduct of TIMP2 x IGFBP7 and HMGB increased right after RIPC, suggestive of cell cycle arrest as an epithelial defensive mechanism against ischemic insult, however, in 4-24 hours post-op, TIMP2 x IGFBP7 and NGAL were lower in RIPC group compared to control (schematic figure above from eSupplement), indicating less kidney damage.
RIPC has been studied in kidney transplant field as well. The REPAIR trial recruited 406 live donor-recipient pairs and looked into 12-month post-transplant eGFR with or without early or late RIPC for both donors and recipients. The result was not significant, but as Zarbock et al. pointed out in their article, it could be due to differences in study protocols, confounding comorbidities, or surgical technique. Further studies to explain the mechanism of protection is warranted and it might be no exaggeration to say that RIPC would be a standard pre-op protocol for cardiac surgery in the near future. Are your kidneys ready for surgery?
Naoka Murakami

No comments:
Post a Comment
Renal Fellow Network encourages comments and discussion regarding the posts. Do not post any comments that are commercial or advertising in nature. Posts will be deleted if commercial or advertising comments are made. Internet users commenting on the Renal Fellow Network must post information which is true and correct to their knowledge. Sources to health/medical claims must be provided when relevant. Moderators reserve the right to erase, without notification, any comment they would judge inappropriate.