Thursday, December 17, 2015
Stop-IgA: Immunosuppression for proteinuric IgA Nephropathy
Monday, November 17, 2014
Michelle P Winn Endowed Lectureship, ASN 2014
Michelle did her undergraduate studies at the University of North Carolina before going to medical school at East Carolina University. She then entered Duke University for residency and fellowship before joining the Duke faculty. Despite spending most of her career at Duke she remained a true Tar Heel (UNC) fan!
She received her training in classical human genetics from Drs Jeffery and Peggy Vance at the Duke Center for Human Genetics. In collaboration with another longtime friend and collaborator and early mentor at Duke, Dr Peter Conlon, Michelle began investigating the genetic heterogeneity of FSGS.
- Together Drs Winn and Conlon collected what is now one of the largest Familial FSGS datasets in the world.
- Michelle’s early work linked familial FSGS in one large family from New Zealand to a locus on chromosome 11.
- Following this she identified TRPC6 as the cause for FSGS in this family. This was a seminal paper published in Science and introduced an ion channel and calcium into the burgeoning field of podocyte biology.
- Michelle’s further work on TRPC6 made a huge contribution to the understanding of the biology of TRPC6 in kidney disease.
- She described linkage of a gene causing MPGN type III,
- identified TNXB mutations causing vesicoureteral reflux,
- was involved in studies of genetic factors influencing the development and progression of IgA nephropathy
- a hybrid CFHR3-1 gene causing familial C3 glomerulopathy.
- Her work also helped to define the disease burden and impact of other FSGS causing genes such as INF2, NPHS2 and PLCe1.
- She discovered Anillin a new gene causing FSGS,
- a new mutation in the WT1 gene
- added further insights into the function and regulation of TRPC6 in podocytes.
Wednesday, June 5, 2013
Treatment of IgA Nephropathy - Update
As the authors point out, one of the major difficulties in determining the best treatment (and assessing the comparative effectiveness of therapies) is the heterogeneity in the presentation and prognosis of patients with IgA. It is extremely common, with up to 1.6% of zero-hour allograft biopsies having evidence of asymptomatic IgA. As a result, many patients are diagnosed incidentally and never have any clinically significant disease. One important issue relates to determining who is going to progress. The recently introduced MEST classification came about in an effort to define histological markers in IgA that predict progression. However, follow-up studies have indicated that the only consistent marker of progression was the degree of interstitial fibrosis and atrophy. It should be noted that this classification does not include crescents which are associated with a poor prognosis. Traditional clinical markers of progression include hypertension, increased BMI, smoking and, most importantly, persistent proteinuria of >1g/24 hours.
The treatment of IgA depends on the clinical presentation. Patients with normal blood pressure, normal renal function and no proteinuria can generally be watched in the clinic with no specific treatment and, in fact, it is debatable if these patients should be biopsied in the first place. The figure below (originally from JASN and reproduced in NRN) provides a suggested algorithm for the management of patients with IgA depending on the stage at presentation.
It is important to state that the only treatment that has been consistently been shown to be beneficial in patients with IgA is RAAS blockade.The role of corticosteroids is controversial and the current KDIGO guidelines suggest the use of steroids only in patients who have been on optimal therapy for 3-6 months, have persistent proteinuria >1g and have an eGFR of >50 ml/min/1.73m2. Low dose steroids are of no benefit and the use of higher dose steroid regimens is associated with significant morbidity so this recommendation comes with significant caveats. Other immunosuppressants including cyclophosphamide, MMF and azathioprine have been trialed in IgA and despite some encouraging results in open-label and retrospective studies, prospective studies have failed to show a consistent benefit. However, there are ongoing RCTs that will be reported in the next 12-24 months that may finally give us the definitive answer with regard to these agents.
Tonsillectomy, more commonly performed in Japan, is not recommended, either by these authors or in the KDIGO guidelines. Fish Oil may be of benefit in patients with persistent proteinuria >1g but is probably of limited use in other groups. One of the limitations of the studies of fish oil in IgA is that they were generally performed prior to the widespread use of ACEi and it is uncertain if they add any additional benefit to these agents. Again, the dose needs to be sufficient (supranormal doses).
Finally, crescentic IgA is a different entity that generally is associated with rapid progression. It is only diagnosed when more than 50% of glomeruli have crescents; the presence of a single crescent in one glomerulus should not prompt the institution of aggressive immunosuppressive therapy. Again, there are no RCTs that demonstrate a benefit of cyclophosphamide but there are some retrospective studies that have shown some effectiveness. That said, in the presence of rapidly progressive disease and active glomerular inflammation, the recommendation is that a combination of steroids and cyclophosphamide should be used.
Friday, November 9, 2012
Image of the Month - GN with a twist
A high power view of a typical glomerulus revealed mesangial expansion and proliferation with normal-appearing capillary loops. There were no cellular crescents and some glomeruli had evidence of focal sclerosis.
Not unexpectedly, the EM found extensive mesangial deposits with no sub-endothelial or subepithelial deposits and a normal appearing basement membrane. The podocyte morphology was also well preserved.
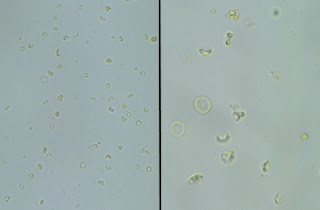
Top on the list of differentials in this patient was IgA nephropathy and as expected, the immunofluorescence revealed extensive mesangial staining for IgA. At this point, many pathology labs would leave it at this and make a straightforward diagnosis of IgA. However, our lab can't just leave it alone and generally also routinely stains for immunoglobulin light chains. Typically in IgA nephropathy, lambda light chains are more prominent than kappa light chains on IF but the difference is not marked.
Thursday, October 4, 2012
To biopsy or not to biopsy - IgA
 The topic of IgA nephropathy has been discussed in multiple posts here in the past. IgA is the commonest primary GN with a wide variety of presentations and prognoses ranging from isolated hematuria to a rapidly progressive GN. Over the last few years, my practice has been that if I see a patient with isolated hematuria, no adverse family history and minimal proteinuria, I will not biopsy them and reassure them that their chance of progression is very low. This is an approach that has also been supported by previous posters.
The topic of IgA nephropathy has been discussed in multiple posts here in the past. IgA is the commonest primary GN with a wide variety of presentations and prognoses ranging from isolated hematuria to a rapidly progressive GN. Over the last few years, my practice has been that if I see a patient with isolated hematuria, no adverse family history and minimal proteinuria, I will not biopsy them and reassure them that their chance of progression is very low. This is an approach that has also been supported by previous posters.An article and accompanying editorial in this month's JASN would appear to support this approach. This was a retrospective review of the outcomes in 141 patients diagnosed with IgA nephropathy with minimal proteinuria (less than 0.5g) between 1975 and 2008 in 8 Spanish hospitals. During this period there was an aggressive policy in place with a very low threshold for renal biopsy. At the time of biopsy, only 16% were hypertensive while 17.7% had no detectable proteinuria. All patients had a normal eGFR at baseline.
Over a mean follow-up of 9 years, no patients were treated with immunosuppressive agents and 41% were treated with RAAS blockade. 5 patients (3.5%) had an increase of 50% from baseline creatinine while 1 patient had a doubling of creatinine (following pregnancy). 14.9% of patients developed proteinuria (more than 0.5g) while it increased above 1g in 6 patients. The only factor predicting increased proteinuria or an increased creatinine after multivariable analysis was the presence of FSGS (S1 by the Oxford Classification).
These results are very reassuring and for me reinforce the idea that we should not be routinely biopsying patients who present like with isolated hematuria. It is notable that most of the hospitals in this study have stopped this aggressive biopsy policy and it is unlikely that a similar study will be done in the future. However, there is no doubt that they should be followed long term because there is a (small) risk of progression. It should be stated that these results are not necessarily generalizable to other populations - studies in Asian populations have found a much higher rate of progression and the indication for biopsy might be different in this group. It would be interesting to know what the genetic factors underlying this difference in outcomes might be.
Wednesday, July 18, 2012
When IgA-ttacks!
Wednesday, April 27, 2011
NKF Spring Clinical Meeting - IgA
 The NKF Spring Clinical meeting started today in Las Vegas. I thought I’d share of the interesting highlights from some of the talks I’ve attended. This post relates to Dr Appel’s lecture on IgA nephropathy, where he described the recent literature on pathogenesis and treatment and a relatively new classification system called the Oxford-MEST system.
The NKF Spring Clinical meeting started today in Las Vegas. I thought I’d share of the interesting highlights from some of the talks I’ve attended. This post relates to Dr Appel’s lecture on IgA nephropathy, where he described the recent literature on pathogenesis and treatment and a relatively new classification system called the Oxford-MEST system. This classification system was devised at an expert group meeting in England. Pathologists (blinded) retrospectively examined 265 biopsies from adult and paediatric patients with IgA, who had five-year follow up data available. The biopsies were scored on pathological variables and entered into a prediction system based on the follow-up data available. They came up with four features that were strongly predictive of renal outcomes:
M – mesangial hypercellularity; scored 0 or 1
E – endocapillary proliferation; scored 0 or 1
S – segmental glomerulosclerosis; scored 0 or 1
T – tubular atrophy/interstitial fibrosis; scored 0, 1 or 2
A notable absence in this classification system is presence of crescents – the reason why this is not included is simply that in the 265 samples they analyzed, there were too few samples with crescents to make any significant inference about.
Further validation of this score is ongoing in various samples, but it appears to be gaining recognition and popularity and is something we should be aware of.
Thursday, December 23, 2010
What causes IgA Nephropathy?
Monday, May 3, 2010
Isolated microscopic hematuria
 We have had a rush of patients with isolated hematuria in my clinic recently. The question that occupies so much precious time of the nephrologist reared it's head....... 'what are the indications for a renal biopsy'.
We have had a rush of patients with isolated hematuria in my clinic recently. The question that occupies so much precious time of the nephrologist reared it's head....... 'what are the indications for a renal biopsy'.Isolated persistent glomerular hematuria (with dysmorphia) without proteinuria, hypertension or reduced GFR is one of 4 things according to several studies [Caldas et al (1990) Lab Ix; 62:15A. Tiebosch et al (1989) NEJM;320:140]. IgA nephropathy, Alport's Syndrome, Thin Basement Membrane disease or mild glomerulonephritis. Approximately 5% have other diagnoses and a number have a normal biopsy.
Most of these patients have a long term benign course. However many patients with Alport's disease develop progressive renal disease, as do a number of patients with this form of IgA nephropathy. Although thin basement membrane disease is said to be benign, it is not exclusively so and many patient have mutations in Col4a3, Col4a4 genes, similar to Alport patients.
In a pediatric study of Physicians deciding whether to biopsy children for isolated hematuria, only 5% said they would. Further in Pediatric studies where biopsies were performed, only 1 in 39 biopsies for isolated hematuria resulted in a change in management.
It is not always possible from family history to make the diagnosis. However, TBMD is frequently inherited in an AD manner, while Alports syndrome is both autosomal recessive and X-linked (rarely AD). Fewer than 10% of IgA nephropathy patients have an inherited form.
The presence of sterile pyuria might also point to a nephrotoxic cause or a component of interstitial disease and might be taken as a sign of underlying disease activity.
So for patients with isolated persistent hematuria and no clear diagnosis one can either monitor the patients regularly for changes in renal presentation or perform a biopsy.
I would favor performing a renal biopsy only if:
- patient requests for certainty/inform family members/diagnostic curiosity
- Any suggestion from H & P that this might be the early stages of a non-benign disease
- Other atypical features including pyuria.
Wednesday, January 27, 2010
Glomerular Density and Predicting Progression in IgA Nephropathy

IgA nephropathy (IgAN) is an unpredictable beast, and identifying patients who will go on to develop progressive disease can be challenging. The classic predictors of progression, namely heavy proteinuria, CKD, glomerular sclerosis and tubulointerstitial fibrosis, are themselves just markers of advanced disease. There is a real need for better early histopathologic predictors of renal prognosis.
One promising prospect is glomerular density (GD), i.e. the number of nonsclerotic glomeruli per mm2, which was the focus of this recent study from Japan. The investigators performed a retrospective analysis of almost 100 IgAN cases with preserved renal function at the time of biopsy (average GFR 90 ml/min). Interestingly, they found that the GD varied hugely between patients, from 1 to 8 glomeruli per mm2. In multivariate analysis, only GD, and the presence of a cellular/fibrocellular crescent, were found to be significant predictors of progression. Patients with a low GD experienced more rapid decline in renal function, and this enhanced risk for progression was increased if a cellular/fibrocellular crescent was also present. Interestingly, the classic predictors of progression listed above did not predict prognosis, presumably due to the early stage of disease.
Of course, these findings will need to be replicated in other ethnic groups. Nonetheless, when a case of IgAN next appears at your biopsy conference, you should pipe up “what’s the GD?”. Just try not to look too smug when you do it.
Thursday, December 17, 2009
IgA Nephropathy Treatment Poll Results
 This week's RFN Poll question is a fun one: let's assume Obama's stimulus package includes in its budget funding for a "Mount Rushmore of Nephrology" to be built. This gigantic statue will feature the faces of 4 prominent nephrologists etched into the rock face of a majestic mountain, preferably at one of the national parks in the Western United States. Of all the prominent nephrologists, which four would you choose as being the most influential in the field? Choose from the list of historic figures listed, and feel free to include "write-in votes" under the "comments" section if your favorite nephrologist is not listed. The list I made is admittedly biased towards physicians who have been practicing recently enough that the subspecialty has actually been in existence (e.g., not including folks like Hippocrates), and conversely I tended not to include the current heavy hitters of Nephrology, reasoning that the jury is still out on these folks. Realize that this is for fun, and I'm sure I've made several oversights.
This week's RFN Poll question is a fun one: let's assume Obama's stimulus package includes in its budget funding for a "Mount Rushmore of Nephrology" to be built. This gigantic statue will feature the faces of 4 prominent nephrologists etched into the rock face of a majestic mountain, preferably at one of the national parks in the Western United States. Of all the prominent nephrologists, which four would you choose as being the most influential in the field? Choose from the list of historic figures listed, and feel free to include "write-in votes" under the "comments" section if your favorite nephrologist is not listed. The list I made is admittedly biased towards physicians who have been practicing recently enough that the subspecialty has actually been in existence (e.g., not including folks like Hippocrates), and conversely I tended not to include the current heavy hitters of Nephrology, reasoning that the jury is still out on these folks. Realize that this is for fun, and I'm sure I've made several oversights. 
Monday, March 2, 2009
Fish Oil for IgA Nephropathy?
 Unfortunately, other than blockade of the renin-angiotensin system via ACE-inhibitors and angiotensin receptor blockers, there are not a lot of evidence-based treatment options for IgA Nephropathy. One other potential addition to the therapeutic regimen for IgA Nephropathy--depending on how you interpret the data--is fish oil.
Unfortunately, other than blockade of the renin-angiotensin system via ACE-inhibitors and angiotensin receptor blockers, there are not a lot of evidence-based treatment options for IgA Nephropathy. One other potential addition to the therapeutic regimen for IgA Nephropathy--depending on how you interpret the data--is fish oil.Omega-3 fish oil consists of essential fatty acids that cannot be made endogenously but rather must be obtained through diet. These fatty acids include linoleic acid, linolenic acid, EPA (eicosapenaenoic acid) and DHA (docosahexnenoic acid). Over the past few decades there have been multiple attempts to see if omega-3 fatty acids might be beneficial in the treatment of IgA Nephropathy, under the rationale that these fatty acids are known to inhibit the production of cytokines and eicosanoids which are felt to be responsible for glomerular injury. However, the data as to their efficacy is mixed.
The strongest piece of evidence that fish oil is useful in the treatment of IgA Nephropathy comes from the Mayo Clinic-initiated study published in the NEJM in 1994 by Donadio et al. Briefly, this study looked at over 100 patients with IgA Nephropathy and persistent proteinuria, randomizing patients to receive either fish oil or an olive-oil placebo. Over a period of two years, only 6% of patients in the fish oil group displayed an increase of 50% or more in the serum creatinine, whereas 33% of those in the placebo-treated group suffered an increase of 50% or more in the serum creatinine. Subsequent long-term follow-up studies seem to support a permanent benefit in the fish-oil group.
While this is encouraging, other RCTs, such as that performed by the Southwest Pediatric Nephrology Study Group, demonstrated an apparent worsening of renal function in a fish oil-treated group compared to a group treated with either steroids or placebo, though this study was not as large as the Mayo Study. Both studies suffer from the fact that neither group was uniformly treated with ACE-I/ARB, which today would be considered standard-of-care. A meta-analysis in 1997 concluded that if there is a beneficial of fish oil in IgA Nephropathy, its effect is probably mild.
If you are going to use fish oil for the treatment of IgA Nephropathy--and in my young opinion it's probably not a bad idea given the lack of available treatments and the apparently minimal downside to using fish oil--there are a couple of things to keep in mind. First, make sure you prescribe a large enough dose. Most of the clinical trials showing a benefit to fish oil have used doses of between 4-12 grams per day, dividing into two or three doses. Second, there is apparently a significant variability between preparations of omega-3-fatty acids in terms of the ratio of fatty acids; there has also been some concern that some over-the-counter preparations may contain trace heavy metals which, if consumed in megadoses over a prolonged period of time, might cause negative health consequences. This has led some to recommend the use of a prescription-only form of omega-3-fatty acids (and also the formulation used in the Mayo study), originally called Omacor but now being marked under the name Lovaza.
Up To Date recommends that "fish oil can be tried in addition to ACE inhibitors or ARBs in patients with protein excretion >500 to 1000 mg/day, a gradual reduction in GFR, and mild to moderate histologic lesions", but it is not considered essential.
Thursday, February 26, 2009
Interesting Case of Adult Henoch-Schonlein Purpura
 Saw a case in the clinic today of a 40-ish year old woman who was diagnosed about a year and a half ago with Henoch-Schonlein purpura. This is notable in that usually this is a pediatric disease--though as this case illustrates it can certainly affect adults. This particular patient had all three elements of the "classic triad" of HSP: purpuric rash, abdominal pain, and arthritis. In addition, she also experienced renal failure secondary to glomerulonephritis, with a creatinine that had elevated to 2.5mg/dL from a normal baseline and whopping proteinuria with a urine protein:creatinine ratio of >20. Fortunately, with plasma exchange, prednisone, and Cytoxan, her symptoms eventually resolved, and today in the clinic (about 1.5 years after having been initially diagnosed) her creatinine was down to 1.2 mg/dL. The disease appears to lie along the same spectrum as IgA Nephropathy, as renal biopsy of HSP patients is often indistinguishable from that of IgA Nephropathy kidneys: mesangial proliferation with IgA deposits. HSP is best categorized as a vasculitis and it is commonly preceded by an upper respiratory tract infection--it has been linked to Strep infection, viral infection, and even certain medications, though in most cases no underlying etiology causing HSP is identified.
Saw a case in the clinic today of a 40-ish year old woman who was diagnosed about a year and a half ago with Henoch-Schonlein purpura. This is notable in that usually this is a pediatric disease--though as this case illustrates it can certainly affect adults. This particular patient had all three elements of the "classic triad" of HSP: purpuric rash, abdominal pain, and arthritis. In addition, she also experienced renal failure secondary to glomerulonephritis, with a creatinine that had elevated to 2.5mg/dL from a normal baseline and whopping proteinuria with a urine protein:creatinine ratio of >20. Fortunately, with plasma exchange, prednisone, and Cytoxan, her symptoms eventually resolved, and today in the clinic (about 1.5 years after having been initially diagnosed) her creatinine was down to 1.2 mg/dL. The disease appears to lie along the same spectrum as IgA Nephropathy, as renal biopsy of HSP patients is often indistinguishable from that of IgA Nephropathy kidneys: mesangial proliferation with IgA deposits. HSP is best categorized as a vasculitis and it is commonly preceded by an upper respiratory tract infection--it has been linked to Strep infection, viral infection, and even certain medications, though in most cases no underlying etiology causing HSP is identified.
Tuesday, February 10, 2009
The Many Faces of IgA Nephropathy
 Heard a case this morning regarding an elderly white patient who presented with nephrotic syndrome and minimal hematuria. After going through the extensive differential diagnosis, focusing largely on the likely candidates (membranous nephropathy and minimal change disease), the biopsy ultimately showed IgA Nephropathy. Though nephrotic syndrome is an uncommon presentation of IgA Nephropathy, the fact that IgA Nephropathy is relatively common means that IgA Nephropathy actually accounts for about 14% of cases of nephrotic syndrome (in whites--IgA Nephropathy is pretty uncommon in blacks).
Heard a case this morning regarding an elderly white patient who presented with nephrotic syndrome and minimal hematuria. After going through the extensive differential diagnosis, focusing largely on the likely candidates (membranous nephropathy and minimal change disease), the biopsy ultimately showed IgA Nephropathy. Though nephrotic syndrome is an uncommon presentation of IgA Nephropathy, the fact that IgA Nephropathy is relatively common means that IgA Nephropathy actually accounts for about 14% of cases of nephrotic syndrome (in whites--IgA Nephropathy is pretty uncommon in blacks). There are a lot of different ways IgA Nephropathy can present. Here are some of them:
1. Asymptomatic hematuria: a lot of cases are picked up with routine urinalyses. Often these cases have little to no progression of renal disease over several decades.
2. Synpharyngitic hematuria: the "classic" presentation of IgA Nephropathy occurs within 1-3 days of a mucosal infection such as a URI.
3. Acute kidney injury: occasionally, IgA Nephropathy will first manifest as AKI. This can take 2 basic forms, and distinguishing between the two of them is critical:
A) The ATN Form: patients may become oliguric as a result of an acute worsening of hematuria, which can result in tubular toxicity, but will almost always recover renal full renal function afterwards.
B) The crescentic Form: patients with crescents on the background of mesangial IgA deposits on renal biopsy have a very poor prognosis and will often progress to permanent renal damage even despite aggressive therapy.
4. Nephrotic Syndrome: as mentioned above, IgA Nephropathy accounts for about 14% of all nephrotic syndrome in whites. This can also take two different forms:
A) "Minimal Change Disease" superimposed on IgA Nephropathy, which tends to be very steroid responsive.
B) "Structural Damage"--severe, prolonged damage to mesangial cells can result in secondary podocyte injury that is generally not reversible and can be thought of as a secondary nephrotic syndrome.
Always keep IgA Nephropathy in mind in formulating a differential diagnosis! It is relatively common compared to a lot of the other glomerular diseases we may invoke.
Sunday, December 28, 2008
Haas System of Classification for IgA Nephropathy
A similar type of system has been developed for IgA Nephropathy known as the Haas system of classification for IgA Nephropathy. Much like lupus nephritis, there is a range of pathologies seen on renal biopsy in patients with IgA Nephropathy, and there is a wide range of prognoses, with many patients going years without any discernable decline in renal function but others which may show a pattern of rapidly progressive glomerulonephritis.
In the Haas paper describing their classification system, the authors took 244 cases of IgA Nephropathy--not including Henoch-Schonlein purpura--and broke down the cases by histologic pattern into 5 subclasses: subclass I (minimal or no mesangial hypercellularity), subclass II (focal and segmental glomerular sclerosis without active cellular proliferation), subclass III (focal proliferative GN), subclass IV (diffuse proliferative GN), and subclass V (any biopsy showing >40% globally sclerotic glomeruli or >40% cortical tubular atrophy or loss). The classification is useful in the sense that there was a statistically significant correlation between IgA subclass and renal survival (with subclass I having the best prognosis and subclass V having the worst prognosis).
Sunday, October 26, 2008
IgA Nephropathy versus Post-Strep Glomerulonephritis
 IgA Nephropathy & Post-Strep Glomerulonephritis (PSGN) are both relatively common causes of glomerulonephritis which can both be associated with upper respiratory infections. How can you tell them apart?
IgA Nephropathy & Post-Strep Glomerulonephritis (PSGN) are both relatively common causes of glomerulonephritis which can both be associated with upper respiratory infections. How can you tell them apart?One of the most important distinctions can be made in taking a good history: In PSGN, glomerulonephritis typically does not set in until several weeks after the initial infection. In contrast, IgA Nephropathy may present with so-called "synpharyngitic glomerulonephritis"--pharyngitis and glomerulonephritis at the same time.
In addition, PSGN classically presents with hypocomplementemia, and if the patient undergoes a renal biopsy there is evidence of an immune complex-mediated process. In contrast, IgA Nephropathy shows normal serologic values (though IgA levels may be elevated in about a third of patients) and the renal biopsy will show mesangial IgA deposition.
Monday, September 22, 2008
Maladie de Berger
 The history of IgA Nephropathy is notable, in large part due to the many famous names of medicine which are associated with it.
The history of IgA Nephropathy is notable, in large part due to the many famous names of medicine which are associated with it. The disease was first described in 1801 by Heberden (of "Heberden's nodes" fame) in a 5-year old child with abdominal pain, hematuria, and purpura of the legs. Then in 1837, Johann Schonlein and Eduard Henoch built upon these discoveries by further characterizing the disease in pediatric populations. It was not until 1968 that the pathogenic role of IgA depositions was revealed, based on the work of French pathologist Jean Berger (left). Prior to his discovery that mesangial IgA deposits are present in these patients, many had believed IgG to be the sole nephritogenic immunoglobulin. For quite some time, the disease was referred to as "Berger's Disease" (not to be confused with Buerger's Disease, or thromboangiitis obliterans), though it has largely been replaced by IgA Nephropathy in recent times.
Thursday, June 12, 2008
Tonsillectomy for IgA Nephropathy?
 IgA Nephropathy is the most common cause of glomerulonephritis globally. It is especially common in Japan, although some of this prevalence may be due to increased screening (all school children undergo a screening urinalysis as part of their normal workup, and as a result many cases of hematuria which normally would go undetected gets worked up). One of the treatments widely used for IgA Nephropathy there is tonsillectomy.
IgA Nephropathy is the most common cause of glomerulonephritis globally. It is especially common in Japan, although some of this prevalence may be due to increased screening (all school children undergo a screening urinalysis as part of their normal workup, and as a result many cases of hematuria which normally would go undetected gets worked up). One of the treatments widely used for IgA Nephropathy there is tonsillectomy.The idea here is that IgA Nephropathy commonly presents with so-called "synpharyngitic glomerulonephritis"--gross or microscopic hematuria, often with transient renal injury, which coincides with the onset of strep throat. Repeated infections can lead to repeated glomerular injury and eventual renal decline; tonsillectomy would be hypothesized to cut down on the number of episodes of pharyngitis and thereby limit the degree of renal damage. We have one patient in our clinic right now we are presently trying to convince to undergo tonsillectomy; we will see if he heeds our advice.

























