 |
| Image from Radiology Picture of the Day http://www.radpod.org/2007/06/19/xanthogranulomatous-pyelonephritis/ |
Showing posts with label Urology. Show all posts
Showing posts with label Urology. Show all posts
Sunday, November 26, 2017
From the Nate Hellman Unpublished Archive: Xanthogranulomatous Pyelonephritis
Labels:
Nathan Hellman,
urinary tract infection,
Urology
Tuesday, February 15, 2011
Primer on Posterior Urethral Valves
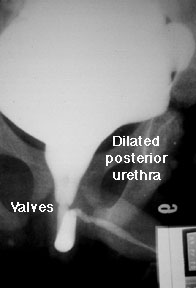 As usually happens when the renal fellows help with the medical student nephrology block, I found myself confronted last week with questions I couldn't answer. One involved the pathophysiology of posterior urethral valves (PUV), which came up in a clinical case. In case there are other fellows who, like me, tend to avoid postrenal conditions in favor of studying more glamorous parenchymal diseases, here is a short primer on PUVS.
As usually happens when the renal fellows help with the medical student nephrology block, I found myself confronted last week with questions I couldn't answer. One involved the pathophysiology of posterior urethral valves (PUV), which came up in a clinical case. In case there are other fellows who, like me, tend to avoid postrenal conditions in favor of studying more glamorous parenchymal diseases, here is a short primer on PUVS.In some senses, the name PUV is a misnomer, since using the word valve implies that there exists a functional valve somewhere, which in this case is dysfunctional. The "valve" in PUV is actually an overgrowth of urethral tissue that forms a membranous barrier to antegrade urine flow. Current thinking is that PUVs form in the embryonic period when there is abnormal integration of the mesonephric ducts into the posterior urethra.
There are three main types of PUVs, of which Type 1 comprises over 95% of cases. Ridges of membrane develop from the floor of the urethra, which then form membranous fins and extend anteriorly. You can see a good illustration of this on the right.
There is some debate as to whether there is a genetic component to this developmental anomaly, but there are no clear inheritance patterns. PUVs occur in boys only, and have an incidence rate of around 1/8,000 male births, but may be more common given increased likelihood of fetal demise. Clinically, they can be picked up on fetal ultrasound, where hydroureteronephrosis, a distended bladder, and a thickened bladder wall in utero can be seen. Postnatal complications include:
-pulmonary hypoplasia (a result of oligohydramnios)
-renal insufficiency, either due to obstructive uropathy or renal dysplasia
-urinary ascites (where high intraluminal pressure causes urine to extravasate from the kidneys)
In older children with a milder clinical course, voiding dysfunction can also be seen.
Definitive diagnosis is by VCUG, where bladder thickening, urethral dilation and severe vesicoureteral reflux are seen. Ultrasound may show hydronephrosis and possibly increased renal echogenicity. Treatment is initially to drain the bladder, and after medical stabilization, valve ablation. Long-term followup with urology, to address issues of chronic voiding dysfunction or incontinence, may be necessary. And for any irreversible kidney damage after relief of obstruction, enter the nephrologists.
Monday, July 5, 2010
Fibroepithelial polyp of the lower urinary tract
I wanted to share a case of a 35-year old man with hypertension and reduced renal function (GFR about 70). Family history was significant for a paternal grandmother and mother with hypertension. No evidence of secondary causes of hypertension including renal artery stenosis, adrenal adenomas, pheochromocytoma, etc. After further questioning a history of urinary frequency was elicited. Ultrasound was done which surprisingly showed bilateral moderate hydronephrosis. Urologic work up included urodynamic studies which showed high bladder pressures and evidence of a bladder outlet obstruction. A cystoscopy showed a possible fibroepithelial polyp (similar to one pictured).
Fibroepithelial polyp of the lower urinary tract is a rare disorder. It usually occurs in pediatric patients but may develop in adults. It is considered non-malignant and treated with a transurethral resection. They usually do not recur. The differential diagnosis also includes a urethelial papilloma and inverted papilloma, both of which are benign but require periodic surveillance for recurrence with cystoscopy. For further reading.
Fibroepithelial polyp of the lower urinary tract is a rare disorder. It usually occurs in pediatric patients but may develop in adults. It is considered non-malignant and treated with a transurethral resection. They usually do not recur. The differential diagnosis also includes a urethelial papilloma and inverted papilloma, both of which are benign but require periodic surveillance for recurrence with cystoscopy. For further reading.
Tuesday, May 18, 2010
Beyond the kidney
Mostly I think about the bladder, in a professional sense, as a possible site for obstruction to be ruled out. Occasionally, when I’m personally reminded about it, I wonder how much urine it can hold. (Pearl from residency: never start a procedure on an empty stomach or with a full bladder) Recently, I had a chance to learn about the bladder while researching an article and discovered several fun facts:
- urine empties into the bladder every 10-15 seconds
- the bladder can hold comfortably between 350-550 cc (12-18 oz) of urine for several hours;
- the urge to urinate usually starts when it has anywhere between 150-300 cc or urine; it can be overridden voluntarily to volumes of 600-800 cc
- speaking of causes of bladder outlet obstruction, the largest bladder stone ever removed (per Guinness world records, 2007 edition) weighed 1.9 kg and measured 17.9 by 12.7 by 9.6 cm
The bladder is able to stretch to accommodate such swings in urine volume thanks to two properties of its epithelium. The first one is a folded apical membrane, which unfolds as the bladder is filling, changing the shape of the top layer of urothelial cells – also called umbrella cells -- from a rounded one to a more flat, squamous one. The second feature is a collection of membrane vesicles, tethered close to the apical surface by cytoskeletal fibrils. As the cell stretches and becomes flatter, the vesicles fuse with the apical membrane, increasing its surface.
The bladder is normally impermeable to the components of urine: molecules, such as urea, ammonia, and water, which usually freely travel through epithelial membranes. Aside from the presence of tight junctions between cells, this impermeability is a function of the composition of the lipid bilayer of the apical epithelial membrane, where the specific arrangement of lipid hydrocarbon tails impairs travel of these molecules across the bilayer. In addition, special proteins, called uroplakins, form aggregates called plaques. These plaques occupy 70-90% of the surface of each cell and help keep urea and water out. When uroplakin was knocked out in mice, their urothelium became permeable to urea, and, to a lesser extent, water.
Interestingly, the urothelium has amiloride-sensitive ENaC–type channels, present at very low levels in normal human bladders (and with different subunit stoichiometry in different mammals). Channel expression may increase in states of elevated bladder pressure, such as in bladder obstruction, an observation consistent with a recent report suggesting that the role of the ENaC -type channels appears to be more important in mechanosensation.
Some interesting reviews and relevant articles can be found here, here, here and here.
Posted by Marta Hristova, MD, PhD
- urine empties into the bladder every 10-15 seconds
- the bladder can hold comfortably between 350-550 cc (12-18 oz) of urine for several hours;
- the urge to urinate usually starts when it has anywhere between 150-300 cc or urine; it can be overridden voluntarily to volumes of 600-800 cc
- speaking of causes of bladder outlet obstruction, the largest bladder stone ever removed (per Guinness world records, 2007 edition) weighed 1.9 kg and measured 17.9 by 12.7 by 9.6 cm
The bladder is able to stretch to accommodate such swings in urine volume thanks to two properties of its epithelium. The first one is a folded apical membrane, which unfolds as the bladder is filling, changing the shape of the top layer of urothelial cells – also called umbrella cells -- from a rounded one to a more flat, squamous one. The second feature is a collection of membrane vesicles, tethered close to the apical surface by cytoskeletal fibrils. As the cell stretches and becomes flatter, the vesicles fuse with the apical membrane, increasing its surface.
The bladder is normally impermeable to the components of urine: molecules, such as urea, ammonia, and water, which usually freely travel through epithelial membranes. Aside from the presence of tight junctions between cells, this impermeability is a function of the composition of the lipid bilayer of the apical epithelial membrane, where the specific arrangement of lipid hydrocarbon tails impairs travel of these molecules across the bilayer. In addition, special proteins, called uroplakins, form aggregates called plaques. These plaques occupy 70-90% of the surface of each cell and help keep urea and water out. When uroplakin was knocked out in mice, their urothelium became permeable to urea, and, to a lesser extent, water.
Interestingly, the urothelium has amiloride-sensitive ENaC–type channels, present at very low levels in normal human bladders (and with different subunit stoichiometry in different mammals). Channel expression may increase in states of elevated bladder pressure, such as in bladder obstruction, an observation consistent with a recent report suggesting that the role of the ENaC -type channels appears to be more important in mechanosensation.
Some interesting reviews and relevant articles can be found here, here, here and here.
Posted by Marta Hristova, MD, PhD
Labels:
bladder,
Marta Hristova,
urinary tract infection,
Urology
Monday, May 10, 2010
"Hey Doc, I think my kidneys hurt."
 How many of you have spoken with patients who complain of mid-back pain and tell you that their kidneys hurt? While dull, aching pain in the mid-lower back is more likely to be associated with musculoskeletal etiologies, kidney-related pain typically presents as sharp, colicky flank pain. Kidney pain usually results from distension of the well-innervated renal capsule due to subcapsular swelling. Specific causes include:
How many of you have spoken with patients who complain of mid-back pain and tell you that their kidneys hurt? While dull, aching pain in the mid-lower back is more likely to be associated with musculoskeletal etiologies, kidney-related pain typically presents as sharp, colicky flank pain. Kidney pain usually results from distension of the well-innervated renal capsule due to subcapsular swelling. Specific causes include:1. Nephrolithiasis. A kidney stone lodged in a ureter or in the kidney parenchyma can obstruct the flow of urine and cause subcapsular swelling and hence, pain. Pain is classically severe, localized to the flank with occasional radiation to the groin, colicky in nature, and may be associated with nausea and vomiting.
2. Pyelonephritis/UTI. Infection and inflammation of the renal parenchyma can also lead to swelling and distension of the renal capsule.
3. Renal masses. This can be in the form of cysts (i.e. polycystic kidney disease) or tumors such as renal cell carcinoma or angiomyolipomas, either of which may distend the renal capsule and cause pain.
4. Renal hemorrhage (intraparenchymal bleeding due to injury or trauma).
5. Hydronephrosis.
6. Renal infarction. A rare cause of kidney pain, this can be due to a thromboembolic event or an in situ thrombosis of the renal artery or its branches. It typically presents with sudden onset, acute flank pain or abdominal discomfort, usually associated with nausea and vomiting. Fever can sometimes be seen as well.
7. Renal vein thrombosis. Can be more insidious or present acutely like renal infarction with sudden onset flank pain.
Thursday, April 29, 2010
Renal Malignancy Syndromes
I had a patient come to see me last week with the rare disorder, Birt Hogg Dube Syndrome (BHD). She was referred with a mildly elevated serum creatinine and microalbuminuria against a background of a single kidney following nephrectomy for renal cancer, which, along with skin abnormalities, is a feature of the syndrome (see left). She initially presented to dermatology with multiple small papule like lesions on the face, which on biopsy were fibrofolliculomas (skin follicle hamartomas). Her renal cancer presented as an incidental finding in 1993 with a 10cm lower pole tumor attached to small bowel. It was removed and pathology was a chromophobe tumor. It has not recurred despite it's large size and local invasion at presentation.
BHD may present with multiple or bilateral renal cancers; it is also associated with oncocytomas of the kidney, and with pulmonary cysts and spontaneous pneumothorax (which she does not have). It is due to a loss of function mutation of a gene on chromosome 17 which may be a tumor suppressor gene and the gene product is folliculin.
We see a lot of patients (relatively) in our clinic with Tuberous Sclerosis Complex, as we are a referral center. TSC is also rarely associated with renal cancer (in 1-2% of cases). There are numerous skin manifestations of TSC, including facial angiomas. Other major manifestations include lymphangiomyomatosis of the lung, cardiac rhabdomyomas, CNS cerebral tubors and renal angiomyolipomas (AML's), as well as renal cysts. It is an autosomal dominant condition. TSC has two genotypes. The gene defect for TSC1 is on Chromosome 9 (encodes for Hamartin); the gene defect for TSC 2 is on Chromosome 16 (encodes for Tuberin). Hamartin and Tuberin are involved in cell cycle regulation.
Finally, Von Hippel Lindau (VHL) is much more frequently associated with renal cell cancer. It is also autosomal dominant with the loss of function defect on chromosome 3 which is also tumor suppressor gene. VHL is associated with
BHD may present with multiple or bilateral renal cancers; it is also associated with oncocytomas of the kidney, and with pulmonary cysts and spontaneous pneumothorax (which she does not have). It is due to a loss of function mutation of a gene on chromosome 17 which may be a tumor suppressor gene and the gene product is folliculin.
We see a lot of patients (relatively) in our clinic with Tuberous Sclerosis Complex, as we are a referral center. TSC is also rarely associated with renal cancer (in 1-2% of cases). There are numerous skin manifestations of TSC, including facial angiomas. Other major manifestations include lymphangiomyomatosis of the lung, cardiac rhabdomyomas, CNS cerebral tubors and renal angiomyolipomas (AML's), as well as renal cysts. It is an autosomal dominant condition. TSC has two genotypes. The gene defect for TSC1 is on Chromosome 9 (encodes for Hamartin); the gene defect for TSC 2 is on Chromosome 16 (encodes for Tuberin). Hamartin and Tuberin are involved in cell cycle regulation.
Finally, Von Hippel Lindau (VHL) is much more frequently associated with renal cell cancer. It is also autosomal dominant with the loss of function defect on chromosome 3 which is also tumor suppressor gene. VHL is associated with
- Hemangioblasomas of the brain, retinal angiomas
- Pheochromocytoma
- Pancreatic neuroendocrine tumors
- Renal cysts
- Renal cell cancer - usually a clear cell cancer
Labels:
Conall O' Seaghdha,
renal cell carcinoma,
Urology
Friday, January 1, 2010
History of Cystoscopy
I stumbled across a bit of Nephrology/Urology history the other day while strolling around a hospital in Paris: this plaque commemorating one of the key steps in the invention of ureteroscopy and cystoscopy. The plaque can be found at Hopital Necker-Enfants Malades, a large hospital now especially renowned for the treatment of pediatric illnesses (and also happens to be the birthplace of the stethoscope by Laennec in 1816).
 A free article on the Development of the Modern Cystoscope via Medscape can be found here. The French instrument described above was not the first attempt at endoscopy, but was apparently one of the earliest. It is described as a "long metal channel through which a mirror reflected light from a petroleum-fueled lamp," and could be used to demonstrate the presence of gallstones and kidney stones in some situations. However, one of its major limitations was that the metal heated up pretty quickly and caused significant patient discomfort. I can't imagine being one of the first patient subjects trying out the new, experimental cystoscope...
A free article on the Development of the Modern Cystoscope via Medscape can be found here. The French instrument described above was not the first attempt at endoscopy, but was apparently one of the earliest. It is described as a "long metal channel through which a mirror reflected light from a petroleum-fueled lamp," and could be used to demonstrate the presence of gallstones and kidney stones in some situations. However, one of its major limitations was that the metal heated up pretty quickly and caused significant patient discomfort. I can't imagine being one of the first patient subjects trying out the new, experimental cystoscope...
 A free article on the Development of the Modern Cystoscope via Medscape can be found here. The French instrument described above was not the first attempt at endoscopy, but was apparently one of the earliest. It is described as a "long metal channel through which a mirror reflected light from a petroleum-fueled lamp," and could be used to demonstrate the presence of gallstones and kidney stones in some situations. However, one of its major limitations was that the metal heated up pretty quickly and caused significant patient discomfort. I can't imagine being one of the first patient subjects trying out the new, experimental cystoscope...
A free article on the Development of the Modern Cystoscope via Medscape can be found here. The French instrument described above was not the first attempt at endoscopy, but was apparently one of the earliest. It is described as a "long metal channel through which a mirror reflected light from a petroleum-fueled lamp," and could be used to demonstrate the presence of gallstones and kidney stones in some situations. However, one of its major limitations was that the metal heated up pretty quickly and caused significant patient discomfort. I can't imagine being one of the first patient subjects trying out the new, experimental cystoscope...
Tuesday, November 3, 2009
The Uroplakins
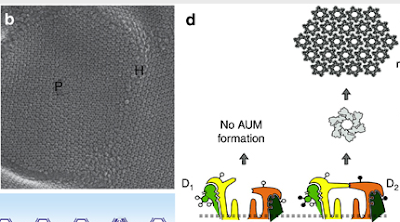
We are taught that water is freely diffusable via cell membranes--even in the absence of aquaporin function, there are usually some water molecules which traverse the lipid bilayer. However, there are tissues within the human body which must be extraordinarily tight: two that come to mind are the thick ascending limb of the nephron, as well as the bladder epithelium. How does the epithelium comprising these "water-tight" barriers obtain these characteristics?
The epithelium lining the bladder (a.k.a. "the urothelium") is one of the tightest epithelia in the body: the bladder must be capable of holding urine for long periods of time without leakage, and furthermore serves as an important barrier for toxic substances filtered by the kidney. The urothelium's water-impermeable properties can be explained in large part by a family of proteins called the uroplakins. The uroplakins form tiny, hexagonal arrays of particles--visualized best by electron microscopy (see figure taken from this excellent recent KI review by Wu et al)--which comprise structures called "urothelial plaques" that overlie the plasma membrane of superficial umbrella cells of the urothelium. It is thought that these plaques are tethered to the lipid bilayer, limiting the movement of phospholipids and therefore limiting water permeability. Interestingly, mice deficient in uroplakins show increased water permeability.
The uroplakins also appear to play a role in urinary tract infections; the uroplakin Ia/Ib glycoprotein is the means by which some strains of E. coli adhere to the urothelium.
Tuesday, July 21, 2009
Caveats for Using Renal Ultrasound to Diagnose Post-Renal Failure
 Most would agree that the renal ultrasound is an invaluable tool in the workup of acute kidney injury. Although the renal ultrasound can give information regarding kidney echogenicity and presence of renal cysts, by and large its predominant utility is in determining the presence or absence of hydronephrosis, a marker for obstructive renal failure ("post-renal" failure when referring to the Holy Trinity of "pre-renal", "intrinsic renal", and "post-renal" categories of AKI).
Most would agree that the renal ultrasound is an invaluable tool in the workup of acute kidney injury. Although the renal ultrasound can give information regarding kidney echogenicity and presence of renal cysts, by and large its predominant utility is in determining the presence or absence of hydronephrosis, a marker for obstructive renal failure ("post-renal" failure when referring to the Holy Trinity of "pre-renal", "intrinsic renal", and "post-renal" categories of AKI). However, there are important caveats to the use of the renal ultrasound to effectively rule-in or rule-out obstructive nephropathy. For instance, false-negatives (e.g., the renal ultrasound does not show hydronephrosis, but there actually is) can occur in the following scenarios:
1. very early obstruction: truly acute obstruction (e.g., with a kidney stone, for instance) may take some time to develop enough distension of the collecting system to detect with our current imaging tools.
2. obstruction in the setting of pre-renal failure: volume-depleted kidneys may not demonstrate significant hydronephrosis until after volume resuscitation, which expands the collecting system.
3. large retroperitoneal tumors: tumors which encase the kidneys may cause obstruction but not allow expansion of the collecting system enough to see hydronephrosis.
4. retroperitoneal fibrosis: this can occur in patients with past extensive GU surgery or prior chemotherapy or radiation therapy and can cause mechanical obstruction without allowing expansion of the collecting system.
In addition, false-positives (e.g., the renal ultrasound is read as "hydronephrosis" but this is probably not pathologic) can occur as well, most notably in pregnancy. It is also common that hydronephrosis detected on ultrasound is a chronic, long-standing issue and not the main culprit for the present episode of AKI.
This post is summarized from some basic but well-written handouts by Dr. Joel Topf from Precious Bodily Fluids. Not a bad idea to print these out and go over cases with a medicine resident rotating on the nephrology consult service...
Labels:
acute kidney injury,
Nathan Hellman,
renal imaging,
Urology
Monday, May 11, 2009
Transvaginal Nephrectomy

Recently two separate groups have reported the successful carrying out of the first-ever human transvaginal nephrectomy--one report coming from the Cleveland Clinic and another from Venezuela. The surgery is being developed as an even less invasive surgical approach than laparoscopy to nephrectomy--in the Cleveland Clinic case, for instance, the patient was able to be discharged within 24 hours following the procedure. Transvaginal nephrectomy is one of several procedures included in the evolving and acronymed field of NOTES (natural orifice translumenal endoscopy surgery).
Labels:
Nathan Hellman,
transplant nephrology,
Urology
Wednesday, March 4, 2009
Urinary Ascites
 An unusual cause of ascites is urinary ascites: this occurs when there is rupture of either the ureter or bladder, leading to leakage of urine into the peritoneal space. In adults, this is almost always due to either blunt trauma to the abdomen, or iatrogenesis, such as nicking the ureter during an abdominal surgery. While not a common diagnosis to make, urinary ascites should be considered after more usual causes of ascites, such as cirrhosis or nephrotic syndrome, have been excluded. An ascites fluid creatinine:serum creatinine ratio >1.0 is highly suggestive of an intraperitoneal urine leak. The peritoneal fluid is typically bland with few WBCs, unlike the situation in spontaneous bacterial peritonitis.
An unusual cause of ascites is urinary ascites: this occurs when there is rupture of either the ureter or bladder, leading to leakage of urine into the peritoneal space. In adults, this is almost always due to either blunt trauma to the abdomen, or iatrogenesis, such as nicking the ureter during an abdominal surgery. While not a common diagnosis to make, urinary ascites should be considered after more usual causes of ascites, such as cirrhosis or nephrotic syndrome, have been excluded. An ascites fluid creatinine:serum creatinine ratio >1.0 is highly suggestive of an intraperitoneal urine leak. The peritoneal fluid is typically bland with few WBCs, unlike the situation in spontaneous bacterial peritonitis.Creatinine is filtered some across the peritoneal membrane (in fact, this is actually used for versions of the peritoneal equilibration test, used in the titration of dialysis dosing for patients on PD), so it is normal to have some creatinine in the peritoneal fluid. But if the peritoneal creatinine is really high relative to the serum creatinine then it means the urine is draining directly into the peritoneal space. Some type of abdominal imaging (ultrasound, CT scan) is often helpful in terms of diagnosing where along the collecting system a rupture has occurred.
Labels:
Nathan Hellman,
renal and liver disease,
Urology
Monday, February 2, 2009
Schistosomiasis and Renal Disease
 Schistosoma species--also known as blood flukes and bilharzia--can cause some interesting forms of renal disease. Although this is not so common in the United States, it is a very common public health problem in Africa and Asia.
Schistosoma species--also known as blood flukes and bilharzia--can cause some interesting forms of renal disease. Although this is not so common in the United States, it is a very common public health problem in Africa and Asia.Chronic Schistosoma mansoni infection in about 10-15% cases is associated with a glomerulonephritis. The etiology is not entirely clear but there is evidence that both schistosomal antigens and antibodies against them can be found in glomeruli from biopsy specimens. Similar to the WHO Classification System for lupus, there is a classification system for schistosomal glomerulopathy which has been set forth by the African Association of Nephrology (AFRAN), and there is an interestingly wide variety of pathologies which can result:
-Class I is a mesangial proliferative GN, the recovery from which is generally good.
-Class II is an exudative GN which is classically observed in patients who are co-infected with both Schistostoma as well as Salmonella (apparently common in some regions).
-Class III is an MPGN.
-Class IV is a proliferative sclerosing GN. Classes III & IV are the most common and most severe form of the disease, which may present as an FSGS-like nephrotic syndrome. Concomitant liver disease (common with Schistosomiasis) and IgA deposition are also suggested to play important pathogenic roles.
-Class V is an AA amyloidosis secondary to chronic inflammation from Schistosomiasis.
Schistosoma hematobium, in contrast, is associated with bladder cancer, particularly in the Middle East. Individuals with Schistosomal-induced bladder cancer are generally treated with radical cystectomy with lymph node dissection, with possible roles for adjuvant or neoadjuvant chemotherapy which are still being determined.
Friday, January 30, 2009
Renal Complications of ESWL
 Extracorporeal shock wave lithotripsy (ESWL), invented during the 1980s in Germany, uses concentrated pulses of sound waves to break up kidney stones too large to pass on their own into smaller pieces, which will then have a chance to be eliminated in the urine. While this therapy has been an extremely useful and much less invasive tool for urologists to use in the treatment of kidney stones, there are nonetheless some side effects which nephrologists should be aware of.
Extracorporeal shock wave lithotripsy (ESWL), invented during the 1980s in Germany, uses concentrated pulses of sound waves to break up kidney stones too large to pass on their own into smaller pieces, which will then have a chance to be eliminated in the urine. While this therapy has been an extremely useful and much less invasive tool for urologists to use in the treatment of kidney stones, there are nonetheless some side effects which nephrologists should be aware of. For instance, the trauma-induced by ESWL sound waves upon thin-walled vessels in the kidney can lead to microscopic hemorrhage, which later results in an influx of inflammatory cells and can potentially result in significant renal scar tissue if the exposure is great enough. This would be most likely to occur in patients who have multiple rounds of ESWL for recurrent stones. Interestingly, there is an emerging literature demonstrating that ESWL is associated with increased (though mild) diastolic hypertension, suggesting that this renal damage could be significant, and biomarkers of renal damage have been demonstrated to be elevated immediately post-ESWL. In addition to these complications, there are others. "Steinstrasse" is a German term (translated as "stone street") describing the post-ESWL accumulation of multiple small stone fragments, which may plug up the ureter and result in obstruction. Hematuria, either gross or microscopic, is relatively common for a few days following the procedure. Finally, bacterial sepsis and its resultant complications (due to translocation of bacteria in the bladder into the bloodstream during ESWL-induced damage to these tissues) can also result.
Wednesday, January 7, 2009
Xanthogranulomatous pyelonephritis
 Xanthogranulomatous pyelonephritis (XGP) is a rare but severe complication of chronic UTIs. I think of it (in simplistic terms) as a pyelonephritis so severe that it results in loss of renal function of the affected kidney as well as being a severe intra-abdominal abscess which can spread to other tissues. In fact, the disease is sometimes referred to as a "pseudotumor" in that it has the ability to "metastasize" to other tissues and often has the radiographic appearance of a renal cell carcinoma on imaging studies. Treatment involves iv antibiotics and very often requires urgent nephrectomy, meaning that a Urology consult should be on-board as early on as possible. Most cases of XGP are unilateral and thought to be secondary to chronic urinary tract infection, often associated with staghorn calculi and chronic obstruction. The most common organisms causing XGP are E. coli, Proteus, and Pseudomonas. Histologically, XGP demonstrates lipid-laden foamy macrophages on a background of diffuse renal parenchymal necrosis.
Xanthogranulomatous pyelonephritis (XGP) is a rare but severe complication of chronic UTIs. I think of it (in simplistic terms) as a pyelonephritis so severe that it results in loss of renal function of the affected kidney as well as being a severe intra-abdominal abscess which can spread to other tissues. In fact, the disease is sometimes referred to as a "pseudotumor" in that it has the ability to "metastasize" to other tissues and often has the radiographic appearance of a renal cell carcinoma on imaging studies. Treatment involves iv antibiotics and very often requires urgent nephrectomy, meaning that a Urology consult should be on-board as early on as possible. Most cases of XGP are unilateral and thought to be secondary to chronic urinary tract infection, often associated with staghorn calculi and chronic obstruction. The most common organisms causing XGP are E. coli, Proteus, and Pseudomonas. Histologically, XGP demonstrates lipid-laden foamy macrophages on a background of diffuse renal parenchymal necrosis.
Sunday, September 7, 2008
UPJ Obstruction
 UPJ obstruction is another common congenital abnormality which under some circumstances can lead to significant renal scarring and chronic kidney diseases. About 50% of ultrasounds during pregnancy which detect antenatal hydronephrosis turn out to have UPJ obstruction.
UPJ obstruction is another common congenital abnormality which under some circumstances can lead to significant renal scarring and chronic kidney diseases. About 50% of ultrasounds during pregnancy which detect antenatal hydronephrosis turn out to have UPJ obstruction. UPJ obstruction is defined as any blockage of urine flow from the renal pelvis to the proximal ureter. The subsequent back pressure within the pelvis can lead to dilatation of the renal collecting system and, if left untreated, can lead to permanent renal damage.
Children with UPJ obstruction typically present with pain, hematuria, recurrent UTIs, failure to thrive, and palpable mass--however, with the increased use of ultrasound, it is not uncommon now to make the diagnosis with routine ultrasound.
UPJ obstruction is a relatively non-specific diagnosis: an anatomical obstruction here can occur due to several reasons: scarring of ureteral valves due to recurrent UTIs, ureteral hypoplasia or abnormal insertion of the ureter into the renal pelvis which might occur as a result of congenital problems of kidney development, and fibrosis following surgery for stone disease are all possible etiologies for UPJ obstruction.
Saturday, September 6, 2008
Horseshoe Kidney versus Crossed Fused Ectopia
 Horseshoe kidney is a relatively common (1 in 400 live births) congenital malformation of the kidney in which the kidneys are fused together. 90% of the time the fusion occurs at the lower poles (upper left photo) and the isthmus (the tissue connecting the two poles) is comprised of either renal parencyhmal tissue or fibrous tissue. In humans, renal development begins during the 4th gestational week, and presumably errors during this process can lead to horseshoe kidney. In the majority of cases, patients are asymptomatic; however, the anatomic abnormalities may be associated with a more complex developmental syndrome OR may result in urologic abnormalities (e.g. reflux nephropathy) that causes CKD. In addition, there is some evidence that some renal tumors (e.g., Wilms' Tumor) may occur with increased frequency in patients with these congenital abnormalities.
Horseshoe kidney is a relatively common (1 in 400 live births) congenital malformation of the kidney in which the kidneys are fused together. 90% of the time the fusion occurs at the lower poles (upper left photo) and the isthmus (the tissue connecting the two poles) is comprised of either renal parencyhmal tissue or fibrous tissue. In humans, renal development begins during the 4th gestational week, and presumably errors during this process can lead to horseshoe kidney. In the majority of cases, patients are asymptomatic; however, the anatomic abnormalities may be associated with a more complex developmental syndrome OR may result in urologic abnormalities (e.g. reflux nephropathy) that causes CKD. In addition, there is some evidence that some renal tumors (e.g., Wilms' Tumor) may occur with increased frequency in patients with these congenital abnormalities.
 In contrast, crossed fused ectopia involves both fused kidneys which lie on one side of the spine, and the ureter of the crossed kidney crosses the midline in order to enter the bladder (lower left photo).
In contrast, crossed fused ectopia involves both fused kidneys which lie on one side of the spine, and the ureter of the crossed kidney crosses the midline in order to enter the bladder (lower left photo).
Sunday, August 3, 2008
Urinoma
Time for some "Renal Radiology Rounds."
The case involves a 77 year-old man with a history of severe benign prostatic hypertrophy. He had been advised to have a TURP in the past but had repeatedly declined. He was hospitalized for nausea, vomiting and R flank pain without hematuria occurring over a week's time, and it was noted that his creatinine had elevated from its baseline of 1.3 to 7. A CT scan on arrival showed the following:
Uploaded on authorSTREAM by nathanhellman
This patient had developed a R-sided urinoma, which is simply a collection of urine which results from rupture of the collecting system due to high pressures from obstruction. It is more typically seen in renal transplant patients post-operatively at the site of the surgical anastamosis between the recipient and donor collecting systems; non-surgical cases of urinomas such as this one are more rare. The patient had a decompressive Foley catheter placed and an IR drain placed to remove the fluid collection. The fluid's creatinine level was higher than serum level, indicating urine as the source. He experienced a post-obstructive diuresis with a lowering of his creatinine following these interventions.
The case involves a 77 year-old man with a history of severe benign prostatic hypertrophy. He had been advised to have a TURP in the past but had repeatedly declined. He was hospitalized for nausea, vomiting and R flank pain without hematuria occurring over a week's time, and it was noted that his creatinine had elevated from its baseline of 1.3 to 7. A CT scan on arrival showed the following:
Uploaded on authorSTREAM by nathanhellman
This patient had developed a R-sided urinoma, which is simply a collection of urine which results from rupture of the collecting system due to high pressures from obstruction. It is more typically seen in renal transplant patients post-operatively at the site of the surgical anastamosis between the recipient and donor collecting systems; non-surgical cases of urinomas such as this one are more rare. The patient had a decompressive Foley catheter placed and an IR drain placed to remove the fluid collection. The fluid's creatinine level was higher than serum level, indicating urine as the source. He experienced a post-obstructive diuresis with a lowering of his creatinine following these interventions.
Labels:
acute kidney injury,
Nathan Hellman,
renal imaging,
Urology
Subscribe to:
Posts (Atom)

















