One of the earliest time-saving tricks I learned as a Nephrology fellow was to always ask the covering housestaff to have a specimen of piping hot urine waiting for me at the time of the initial consult: I was trained to do a urinalysis on all patients on whom I am called to see. While I have been impressed with its usefulness of several occasions, there is surprisingly little standardization for the technique, and not a lot of literature providing objective criteria for diagnosis.
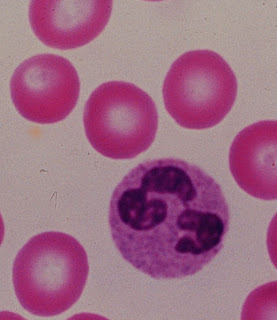
One of the earliest time-saving tricks I learned as a Nephrology fellow was to always ask the covering housestaff to have a specimen of piping hot urine waiting for me at the time of the initial consult: I was trained to do a urinalysis on all patients on whom I am called to see. While I have been impressed with its usefulness of several occasions, there is surprisingly little standardization for the technique, and not a lot of literature providing objective criteria for diagnosis.A recent study in C-JASN by Perazella et al looked at the ability of the urinalysis to distinguish between ATN versus pre-renal AKI on 267 consecutive inpatients with AKI in the Yale-New Haven Hospital system on whom a renal consult was called. Participating nephrologists were asked to assess a cause of either "ATN", "pre-renal", or "other" at two different time points: (1) just after history & physical but before microscopy diagnosis, and (2) after patient discharge or death. As biopsies were not done in this study, the 2nd & final diagnosis--based on clinical judgement--was the "gold standard." The urinalysis itself was carried out in a standardized fashion and a scoring system based on the number of casts or renal tubular epithelial cells (RTECs) was developed.
Not surprisingly, patients with a high "urine sediment score" (indicating many casts or RTECs) had a high rate of ATN as a final diagnosis while those with lower scores were more likely to have pre-renal AKI as a final diagnosis. While this is not groundbreaking, what is worthwhile about this study is that (a) they prove that the urinalysis is a valuable tool for diagnosis by showing that a significant number of patients had their diagnosis changed following urinalysis, and (b) they tackle this problem in a systematic fashion.



















.jpg)