 In
renal transplant recipients with allograft dysfunction, differentiating between a viral infection or
acute cellular rejection as the etiology of interstitial nephritis can be
difficult – especially as they can commonly occur concurrently.
In
renal transplant recipients with allograft dysfunction, differentiating between a viral infection or
acute cellular rejection as the etiology of interstitial nephritis can be
difficult – especially as they can commonly occur concurrently.
We
recently saw a 40-year-old woman who received a deceased donor kidney
transplant less than one year ago who presented with an initial complaint of
gross hematuria and an elevated creatinine (2.2 mg/dL from nadir of 1.4
mg/dL). The allograft ultrasound showed thickening of the urothelium. Prompt
biopsy of the allograft revealed acute cellular rejection (ACR 1B), and she was
treated with high dose steroids and anti-thymocyte globulin.
Over
the next several weeks, she continued to complain of intermittent gross
hematuria. Cystoscopy was unremarkable. One month later she presented with
worsening renal function, cough and shortness of breath. A nasopharyngeal
respiratory viral panel ultimately revealed…adenovirus – which was also then found
both the blood and urine (millions of copies in each). A repeat allograft
biopsy was consistent with adenovirus nephropathy.
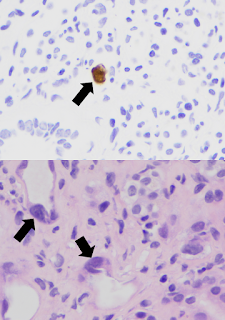
Adenovirus is a double-stranded DNA virus with more than 50 distinct serotypes. Though adenovirus infection is relatively common, adenoviral infection of the renal allograft is rare and also difficult to diagnose if viral inclusions are not present in the biopsy (see image above, black arrows indicating nuclear viral inclusion bodies). Based on a limited number of reported cases, patients typically present with fever, hematuria, dysuria, and acute kidney injury. Adenoviremia and viruria are present, as well as decoy cells similar to those seen with BK virus infection. Though it is possible that this patient may have had only ACR from the beginning (a close re-review of the 1st biopsy revealed no viral inclusions), it’s plausible that the adenovirus was responsible for the gross hematuria and thickened urothelium that were present from the start.
Adenoviral infection usually affects multiple organs and can be life threatening, though some patients are able to clear the virus and recover complete allograft function. After anti-viral treatment with intravenous cidofovir, our patient’s creatinine rose to 9 mg/dL. Unfortunately, she remains dialysis dependent and is undergoing re-evaluation for a second transplant. This challenging case is a reminder that both rejection and infections must be considered when interstitial nephritis – and that one may be a decoy for the other!
Posted by Samira Farouk
Chief Fellow, Division of Nephrology
Icahn School of Medicine at Mount Sinai
















No comments:
Post a Comment