Barry, 62, is under evaluation as a kidney donor to his wife Susan. At his first appointment, you measure his blood pressure at 155/95.
Which one of the following is correct?
A) You should tell Barry that he is ineligible for donation given that he his hypertensive.
B) A single office BP reading is insufficient to make a decision about eligibility.
C) If Barry needs antihypertensive medication, he cannot be a kidney donor.
D) You should counsel Barry that studies show his BP will increase significantly after kidney donation.
Here's how you responded:
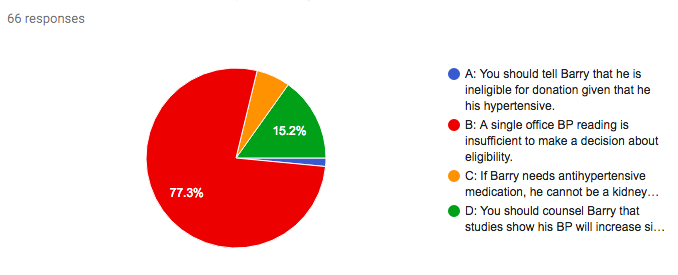
Answer: B.
The impact of kidney donation on blood pressure is not clearly defined. Studies in this area have been limited by small numbers, heterogeneous parameters, and absence of suitable control groups.
While there are several earlier studies without a comparator group, more recent research comparing blood pressure in donors with a matched control group provide more useful information. Ibrahim et al compared 255 donors from their larger Minnesota cohort with a matched control group, and found no statistically significant difference in the proportion of those with blood pressure of 140/90 or higher (14.4% donors vs 18.7% controls). A 2006 meta-analysis examined pooled data for a total of 5145 donors from 9 controlled studies (comparing donors with healthy adults matched for age, sex and ethnicity). A small increase in blood pressure (6mmHg systolic and 4mmHg diastolic) was noted in donors over 10-year follow-up. Finally, a 2015 prospective study of 182 living donors and 171 matched controls found a (very!) small increase in blood pressure (2/1mmHg) after 3 years, with no significant difference between the two groups.
Our knowledge of outcomes for donors with pre-donation hypertension is even more limited. Textor et al reported on 148 Caucasian donors, before and up to 12 months after donation. 24 donors had hypertension at baseline (average ambulatory blood pressure greater than 135/85mmHg, or on antihypertensive treatment). These donors were older and had a higher BMI than normotensive donors. They had normal GFR and no proteinuria, and were treated with both pharmacological and non-pharmacological methods to control blood pressure. There was no significant increase in blood pressures (indeed, a slight decrease), in this very short follow-up period.
There is no clear evidence that kidney donation increases the risk of hypertension in most donors. Higher blood pressure, BMI and age do, however, confer greater risk in potential donors, as in the general population. As recommended by KDIGO Guidelines, pre-donation assessment should involve at least 2 office measurements of blood pressure and, where there’s uncertainty/variability, ambulatory blood pressure monitoring. Where blood pressure can be controlled with 1 or 2 agents, and there is no end-organ damage, hypertension alone is not considered a contraindication to donation. Pre-donation, individualized risk assessment, careful counselling and optimisation of risk factors is essential. Afterwards, close follow-up for management of hypertension and secondary prevention strategies for cardiovascular disease is key.
Don't agree with the answer? Get on twitter and tell us what you think...
Submit your responses for Case 4 now!
Complete the 7-day challenge and you'll have a whole new perspective on Living Kidney Donor Risk and the #NephMadness #TransplantRegion
Don't forget to submit your #NephMadness brackets here
Please note these are fictional cases with open access stock images. They do not represent real cases.
Created by Kate Robson (Nephrologist, Melbourne, Australia and NSMC Intern 2018)
















No comments:
Post a Comment